Nurse Manager Burnout: Recognition and Recovery Strategies
Supporting the leaders who support patient care.
In This Article
The Breaking Point Nobody Talks About
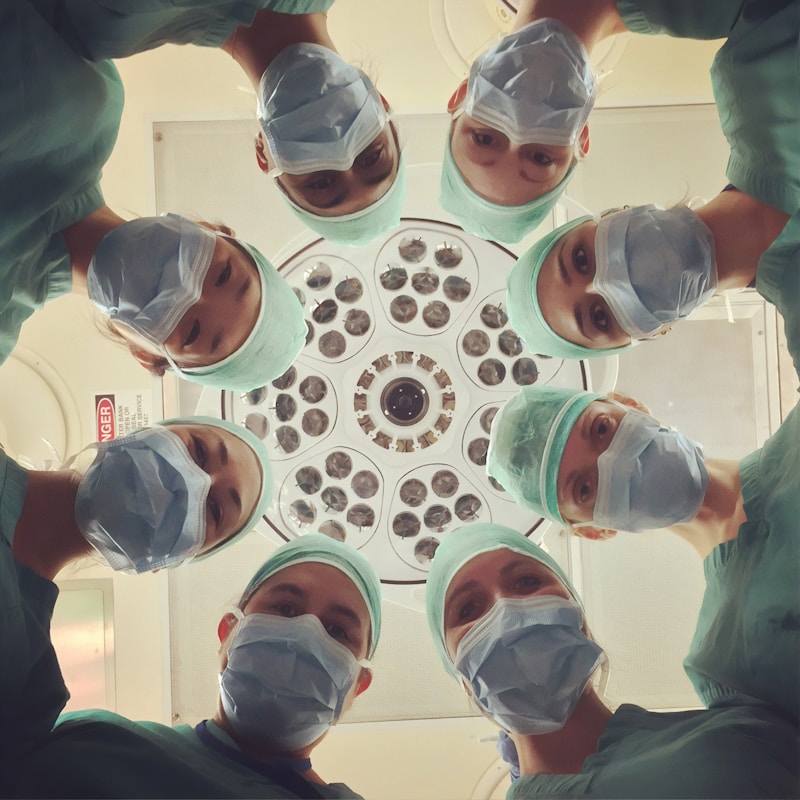
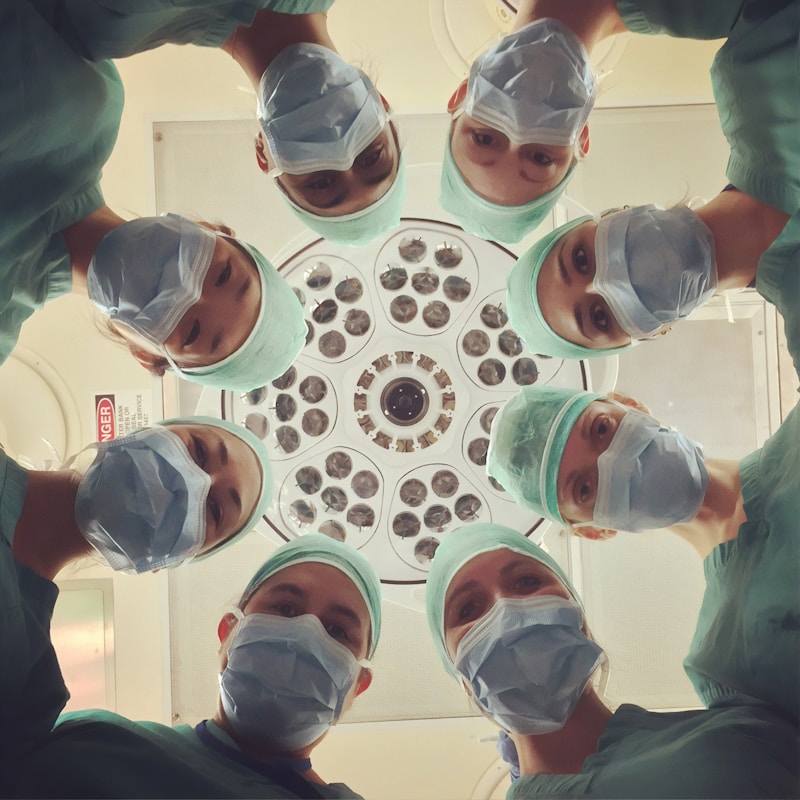
Nurse managers occupy one of the most emotionally demanding positions in healthcare. They absorb stress from every direction: staffing shortages from administration, patient complaints from families, burnout from their nursing staff, and regulatory pressure from compliance teams. Yet the conversation about healthcare burnout rarely focuses on them.
The data tells a stark story. Studies published in the Journal of Nursing Administration found that nurse managers report higher burnout rates than bedside nurses in many healthcare systems. The reasons are structural: they carry clinical accountability, administrative burden, and emotional labor simultaneously, often without the support systems available to direct care staff.
Recognizing and addressing nurse manager burnout is not just a wellbeing issue. It is an operational imperative. When nurse managers burn out, entire units destabilize.
Recognizing the Warning Signs
Nurse manager burnout does not arrive suddenly. It develops through progressive stages that are easy to rationalize away in a culture that celebrates self-sacrifice:
Early indicators:
- Dreading the commute to work when the job used to feel purposeful
- Increasingly short patience with staff questions or requests that previously felt routine
- Difficulty disconnecting from work during off hours, checking emails and messages compulsively
- Physical symptoms: disrupted sleep, persistent fatigue, headaches, or digestive issues that correlate with work cycles
Escalating signs:
- Emotional detachment from staff concerns that previously mattered
- Decision fatigue leading to avoidance or delegation of choices that require judgment
- Cynicism about organizational initiatives or improvement efforts
- Withdrawal from peer relationships and professional development activities
Critical stage:
- Questioning the decision to enter healthcare management entirely
- Making errors in scheduling, budgeting, or compliance documentation that would not have happened previously
- Using sick time not for illness but for mental health recovery
- Considering resignation without a plan, simply to escape
The challenge is that many of these signs mirror the "normal" stress of healthcare management. The difference between manageable stress and burnout is duration and recovery. Stress resolves when the stressor ends. Burnout persists even during time off.
Why Nurse Managers Are Uniquely Vulnerable
Several structural factors make nurse manager burnout distinct from general healthcare burnout:
Span of control. Many nurse managers oversee 50 to 100 or more direct reports across multiple shifts. This ratio exceeds management best practices in virtually every other industry and makes meaningful individual connection nearly impossible.
24/7 accountability. Unlike most management roles, nurse managers are often the escalation point for all shifts. Middle-of-the-night calls about staffing emergencies, patient incidents, or equipment failures erode the recovery time that prevents burnout.
Role ambiguity. Nurse managers are expected to be clinical experts, business managers, HR specialists, compliance officers, and emotional support providers simultaneously. Few receive adequate training in all these domains, creating constant feelings of inadequacy.
Invisible labor. The emotional labor of supporting a nursing staff through patient deaths, workplace violence, and chronic understaffing is rarely acknowledged in performance evaluations or compensation structures. The work is expected but not valued.
Organizational sandwich. Nurse managers translate between executive leadership and bedside staff. They must implement unpopular decisions from above while advocating for resources from below, satisfying neither audience fully.
Recovery Strategies That Actually Work
Burnout recovery for nurse managers requires both individual strategies and organizational support. Individual strategies alone are insufficient when structural problems persist, but they provide essential coping while systemic changes develop.
Individual Recovery
Boundary reconstruction. Burnout often follows the gradual erosion of work-life boundaries. Recovery requires deliberately rebuilding them:
- Establish specific hours when work communication is not checked
- Delegate after-hours escalation to charge nurses for issues that do not genuinely require manager involvement
- Create physical separation between work and personal spaces, especially for those who work hybrid schedules
Professional identity reconnection. Many burned-out nurse managers have lost touch with why they entered the profession. Reconnecting with clinical purpose through:
- Occasional bedside shifts that reconnect with patient care
- Mentoring a new nurse or nursing student
- Attending professional conferences that reignite intellectual engagement
- Reading nursing literature outside of operational requirements
Peer support networks. Other nurse managers are the only people who truly understand the role. Building genuine peer connections through:
- Regular informal meetings with counterparts from other units
- Participation in nurse manager support groups (many health systems now offer these)
- Professional association involvement that connects managers beyond their own organization
Physical recovery. Burnout has physiological components that require physical attention:
- Sleep hygiene improvements that address the disrupted patterns common in healthcare management
- Regular physical activity, even brief walks, that interrupts the stress cycle
- Nutritional attention, as stressed managers often skip meals or rely on caffeine and convenience food
Organizational Support
Individual resilience cannot compensate for organizational dysfunction. Health systems serious about nurse manager retention must address structural contributors:
Span of control reduction. Splitting oversized units or adding assistant managers so that no single manager oversees more than 40 to 50 staff members. This investment pays for itself through reduced manager turnover and improved unit performance.
Administrative support. Providing dedicated scheduling coordinators, administrative assistants, or technology solutions that reduce the clerical burden on nurse managers. Time spent on schedules and spreadsheets is time not spent on leadership.
After-hours coverage models. Establishing nursing supervisor or house supervisor roles that handle overnight and weekend escalation, protecting manager recovery time.
Leadership development. Providing formal training in the business, HR, and management skills that nurse managers need but rarely receive in clinical education.
Mental health resources. Offering confidential counseling services specifically designed for healthcare leaders, not generic EAP programs that may not understand the unique pressures of the role.
Creating a Sustainable Management Practice
Beyond recovery from acute burnout, nurse managers benefit from developing sustainable practices that prevent recurrence:
Energy management. Rather than trying to do everything every day, effective managers identify which activities generate energy (staff development, clinical problem-solving) and which drain it (administrative reporting, conflict resolution). Structuring days to alternate between energy-generating and energy-draining activities creates sustainability.
Delegation development. Many nurse managers struggle to delegate because they believe no one else can do the work adequately. Investing in charge nurse development creates a leadership team that shares the burden and provides growth opportunities for emerging leaders.
Strategic disengagement. Not every organizational initiative requires the same level of engagement. Experienced managers learn to identify which projects genuinely affect their unit and which can receive minimum viable participation.
Regular self-assessment. Building a habit of honest self-evaluation using validated burnout assessment tools helps managers catch developing problems before they reach critical stages.
The Frontline Take
Nurse manager burnout is not a personal failure. It is a predictable consequence of structural demands that exceed human capacity. The healthcare leaders who sustain long, effective careers in management are not simply tougher than those who burn out. They are better supported, more intentional about boundaries, and more willing to ask for help. Health systems that invest in nurse manager wellbeing protect their most critical leadership layer and, by extension, the quality of care their patients receive.
Key Takeaway
Supporting the leaders who support patient care.
Frontline Take
HR's View From The Floor
Related Articles

New Opportunities, New Risks: Using AI to Engage Healthcare Teams Across Shifts and Schedules
Healthcare organizations are turning to AI-powered tools to bridge communication gaps across 24/7 operations—but implementation requires careful attention to burnout, equity, and trust.

Combating Burnout in Frontline Healthcare: A Manager's Playbook
Evidence-based strategies for healthcare leaders to recognize, prevent, and address burnout before it impacts patient care and staff retention.

Leading Through Crisis: Healthcare Supervisor Resilience
Building leadership capacity for the next healthcare emergency.